We are living in the age of AI and with powerful capabilities, it is changing the entire landscape of Insurance. From Policy administration to claims management, AI is not a buzzword but an absolute gamechanger. Gone are the days of delayed claims processing TAT because with Automation in claims management processes, processing claims has become a breeze for insurers. However, are Health insurers steadfast enough to rapidly adapt to AI. Infact, a whopping 60 % of Health insurance claimants have reported experiencing a delay of six to forty eight hours between claims approval and hospital discharge.
Concerning, isn’t it? But a modern-day AI tool like iNube’s AI Quest can help you tackle a similar challenge in Health Claims management like it never existed!
Introducing iNube’s AI Quest………
If the challenge mentioned above strikes a chord with you, then you need to read on to decode some interesting facts that AI-driven solution will help you achieve in Health Claims management.
iNube’s AI Quest is a dedicated labs wing that comprises a team of Insurance and AI experts developing robust AI capabilities across the insurance value chain, that speaks innovation and growth. The seasoned insurance expertise combined with AI enthusiasts has enabled the team to offer you Modern day AI capabilities which is not only the need of the hour but a necessity.
How AI Quest Transforms Health Claims Management?
Our AI Quest is that Modern wizard which has developed modern capabilities for streamlining key tasks in Health claims management. The robust capabilities are developed keeping in mind the intricacies at every stage of the health claims management process.
Here’s a closer look at the modern capabilities that our AI Quest offers:
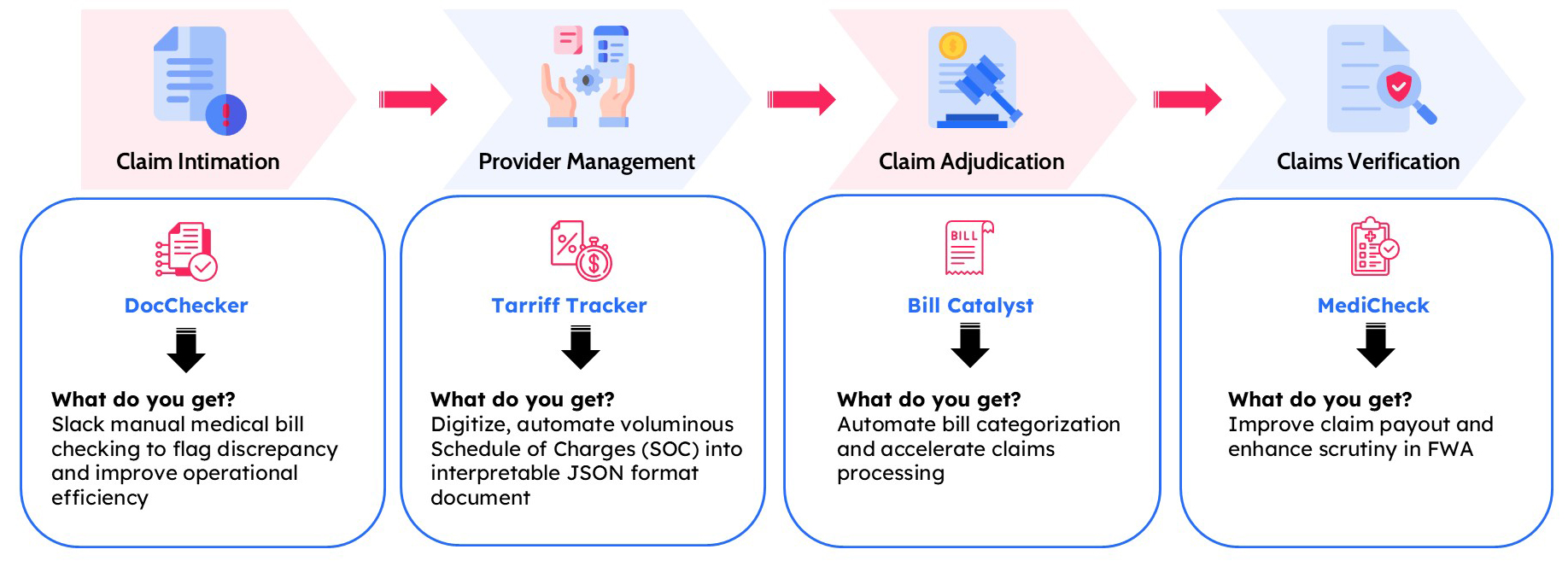
DocChecker
AI Quest’s DocChecker helps in automating one of the key tasks during the claim intimation process. During the reimbursement claims, the policy holder has to upload a multiple number of documents including claims form, ID proofs, payment details and more.
AI Quest’s DocChecker efficiently categorizes all mandated documents uploaded by the insured according to the insurance company’s requirements. It scans through each document, categorizing them accurately and flagging any deficiencies or discrepancies. This ensures that all necessary documents are in order, making the process smooth and efficient for both the insurer and the insured.
Tariff Tracker
This is another one of the key capabilities of iNube’s AI Quest which helps during the provider management stage of Health claims management. AI Quest’s TariffTracker leverages Gen AI to transform complex Schedule of Charges (SOC) data into an easy-to-consume format. It processes and organizes this data into a tabular format for straightforward consumption. The tool digitizes hospital SOCs, speeding up claims adjudication. Additionally, it uses an API-first approach to generate data in JSON or Excel formats, ensuring seamless integration and accessibility.
BillCatalyst
AI Quest’s BillCatalyst uses Gen AI to process and categorize lengthy bills according to IRDAI standards. It identifies bill dates to distinguish between Pre-Hospitalization, Main claim, and Post-Hospitalization bills. The AI extracts information and categorizes bills as per the respective guidelines. Additionally, it provides a summary of all sorted bills, including a grand total of the amount to be paid.
MediCheck
Another one of the key capabilities of iNube’s AI Quest-MediCheck. AI Quest’s MediCheck solves a crucial issue of abuse and leakages in health claims. During health claims processing, especially in reimbursement, there is a potential revenue leakage of the claims that stems from the people claiming for medicines that are not prescribed by the doctors. MediCheck will be manually scrutinizing the data for detecting the discrepancies.
It leverages advanced Gen AI to enhance the detection and flagging of fraudulent health claims. It flags discrepancies in medical bills by comparing them with the prescribed medicines. The AI can read doctors’ handwriting to verify prescriptions and understands trade names and drug compositions to identify discrepancies. It also assesses the quantity of prescribed medicines. Integrated with an API-first approach, it pushes discrepant information to the insurance company for further action.
What Lies for You with These AI Quest Capabilities?
Wondering what lies for you with these modern-day AI Quest capabilities in Health claims management?
Here’s a brief look at what you get with each of these AI Quest capabilities in Health Claims management:
Conclusion
It’s time to go beyond the traditional landscape of Health Claims management and harness the revolutionizing capabilities of AI to turnaround this tedious and manual intesive landscape of Health claims management. The AI Quest capabilities are developed by seasoned industry experts and AI experts that help you get a competitive advantage amidst a surge of AI driven solutions in the market. With modern GenAI technology, each of these capabilities are made for scalability driven by innovation. Streamline health claims management and move beyond operational bottlenecks with iNube’s AI Quest.




